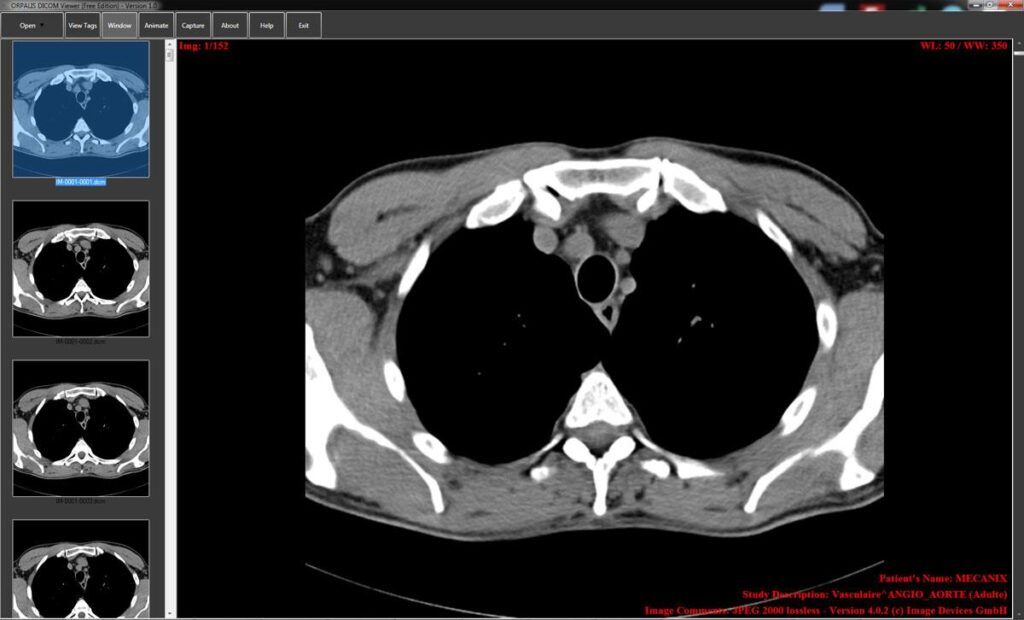
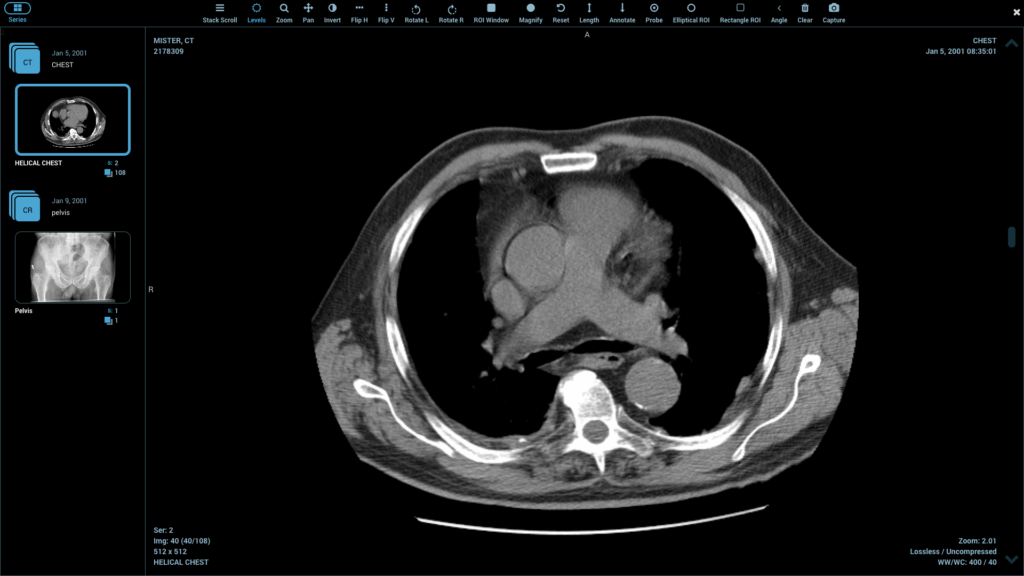
Enhancing the accuracy of your radiology reports is not just about being correct; it’s about providing a clear, actionable story that guides patient care. Inaccurate or unclear reports can lead to delayed diagnoses, unnecessary procedures, and patient anxiety. Think of your report as the critical bridge between your expert analysis and the treating physician. We’re going to walk through practical steps you can take today to make that bridge stronger and more reliable, starting with the technology you use every day. Using a high-quality DICOM medical image viewer is the foundational first step, as it provides the clarity and tools needed for a precise assessment.
Start with a Crystal-Clear Foundation: Your DICOM Viewer
You can’t write an accurate report if you can’t see the details. A robust DICOM viewer is as essential as a sharp microscope is to a pathologist.
Modern viewers go beyond simple display. They offer features that directly contribute to diagnostic confidence. Look for tools like adjustable windowing and leveling to bring out subtle contrast differences, zoom functions for a closer look at fine details, and side-by-side comparison for tracking changes over time. These technical capabilities are your first line of defense against perceptual errors.
A powerful viewer transforms a static image into a dynamic dataset you can explore. Don’t settle for a viewer that feels clunky or limited. The right tool should feel like an extension of your own vision, helping you isolate and interrogate findings with precision.
Master the Art of Structured Reporting
Free-text dictation has its place, but it’s also a common source of inconsistency and missed information. Structured reporting uses standardized templates with specific fields to fill in, acting as a checklist for your analysis.
Why Structure Wins
The benefits are immediate and significant. Structured reports ensure you consistently address all relevant areas for a given study type. This eliminates the “oops, I forgot to mention the adrenal glands” moment. They also create reports that are easier for referring physicians to read quickly, finding the information they need without searching through paragraphs of text.
Consistency is the bedrock of accuracy. By using a template, you build a habit of thoroughness that becomes second nature.
Implementing Templates Without Losing Your Voice
The fear with templates is that they make reports sound robotic. The key is to find a balance. Use the structure for the factual components—like size, location, and density of a lesion—but leave room for a “Impression” or “Conclusion” section where you can use your clinical judgment and write in a more narrative style. This is where you interpret the facts and tell the clinical story.
Cultivate Effective Communication Habits
A report is a form of communication. The most accurate observation in the world is useless if the person reading it misunderstands it.
Be Specific and Unambiguous
Vague language is the enemy of a good report. Compare these two statements:
- Vague: “There is a suspicious lung nodule.”
- Specific: “There is a 8mm spiculated solid nodule in the right upper lobe.”
The second statement gives the referring physician concrete information. They know the size, appearance, and exact location, which directly informs the next steps. Avoid terms like “maybe,” “possibly,” or “likely” unless you are providing a clear differential diagnosis.
Prioritize Your Findings
Don’t just list observations in random order. Start with the most critical finding that needs immediate attention. Follow with clinically significant incidental findings, and then other routine observations. This “triage” approach ensures the most important message is never buried. A busy ER doctor will thank you for making the critical finding impossible to miss.
Double-Check Your Work: The Power of a Second Look
Every radiologist knows the feeling of spotting something on a final review that was missed initially. Building a deliberate review process into your workflow is non-negotiable for accuracy.
The “Fresh Eyes” Technique
If possible, take a short break after interpreting a complex study before finalizing the report. Coming back to it with fresh eyes can help you catch errors or perceive something new. This is especially helpful for studies with a large number of images.
Leverage Peer Review and Collaboration
Don’t work in a silo. If a case is particularly challenging, there is immense value in asking a colleague for a quick consult. A second opinion isn’t a sign of weakness; it’s a sign of professional diligence. This collaborative culture is a hallmark of high-quality radiology practices.
Conclusion: Accuracy as a Continuous Journey
Enhancing report accuracy isn’t a one-time task you check off a list. It’s a continuous commitment to quality that blends technology, standardized processes, and sharp communication skills.
By investing in a superior DICOM viewer, adopting structured reports, and refining how you communicate findings, you build a system that minimizes error and maximizes clarity. Your accurate reports become a trusted resource for your colleagues and, most importantly, lead to better outcomes for the patients who depend on your expertise. Start by auditing one part of your process this week—maybe explore a new feature in your viewer or try a template for one common study type. Small, consistent improvements add up to a major impact.
Frequently Asked Questions
What is the biggest barrier to accurate radiology reporting? Often, it’s a combination of high workload and inefficient tools. Time pressure can lead to shortcuts, while a poor-quality viewer can make it harder to see crucial details. Addressing these systemic issues is as important as individual technique.
How can AI help improve report accuracy? AI tools are emerging as powerful assistants. They can act as a “second set of eyes,” highlighting potential abnormalities you might have missed (like a small fracture) and helping to prioritize cases. However, the final interpretation and responsibility always remain with the radiologist.
Are structured reports really faster? After a short learning curve, yes. While they might feel slower at first, templates eliminate the mental energy spent on how to structure each sentence and ensure you don’t omit key elements, ultimately speeding up the dictation and editing process.
What’s one simple habit I can start today? Implement a final “impression check.” Before you sign the report, re-read your impression section alone. Ask yourself: “If I were the referring doctor, would this be perfectly clear and actionable?” This 10-second habit can catch ambiguities and ensure your main message is on point.
Final Thoughts: Your Report is Your Legacy
In radiology, your report is the primary record of your expertise. It’s what guides treatment and impacts lives long after you’ve moved to the next case. By embracing the right technology, refining your structure, and honing your communication, you transform that document from a simple description into a powerful tool for patient care.
Start small, but start today. Pick one tip from this guide—whether it’s mastering a new feature on your DICOM medical image viewer or creating a template for one frequently used study. Each step you take builds a culture of accuracy that benefits your entire team and, most importantly, your patients.